Your Amazing Cervix
Artwork by Susan Erlich, all rights reserved.
Pinpointing the fertile window is one of the questions that comes up all the time in my practice. Knowing when to have sex for optimal chances of conception is one of the most important, and often most confusing aspects of babymaking. Since January is Cervical Health Awareness month, let’s take a moment to understand how our cervix’ can inform our optimal fertility window, and reduce all of the confusion around how to time sex.
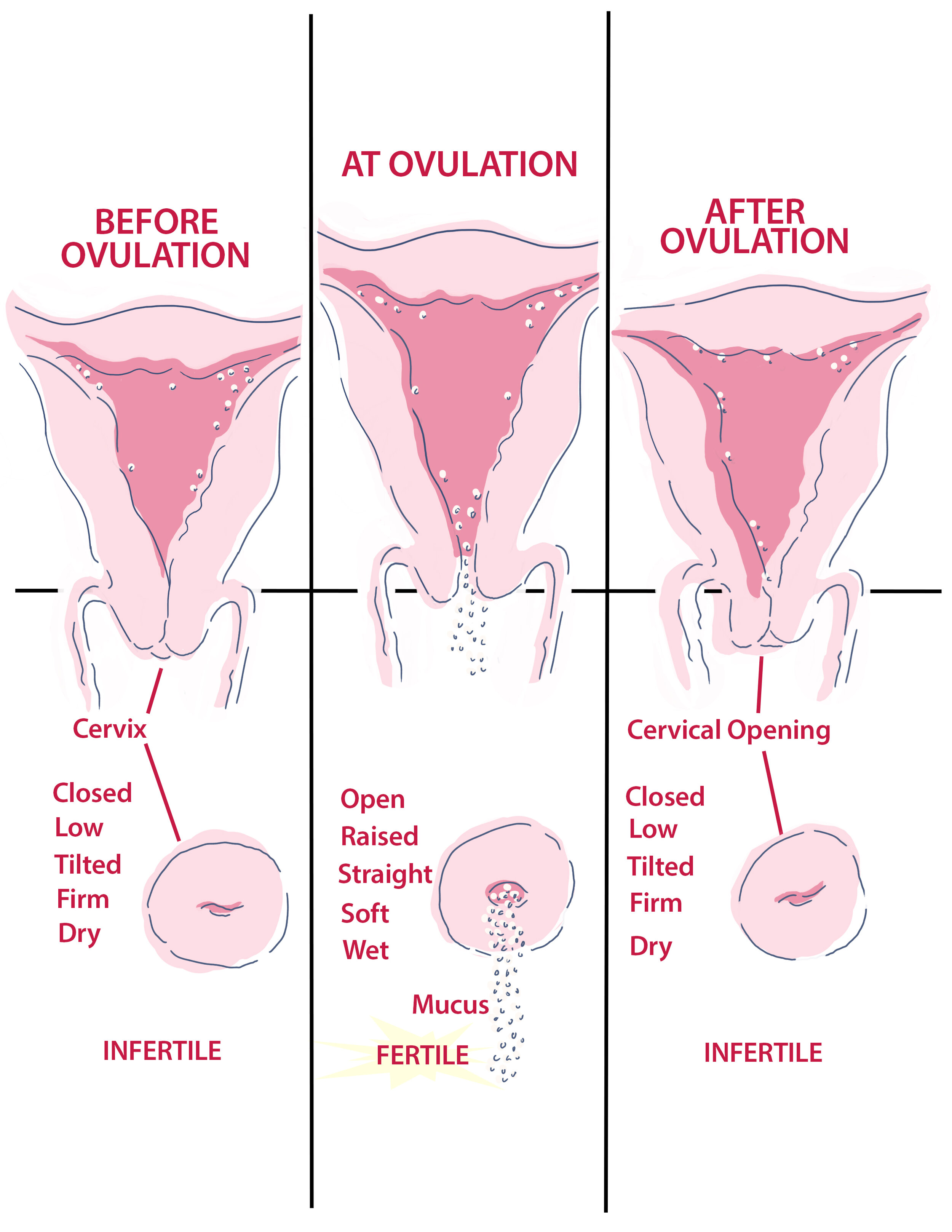
For starters, let's do a quick review of cervical anatomy. The cervix is a structure located at the base of your uterus and is located at the top of the vaginal canal. While the cervix is actually part of the uterus (I like to think of it as the end of a balloon without the knot in it), it is considered its own structure, and it goes through cyclical changes of its own throughout the menstrual cycle. It has a small opening, called the cervical os, which changes is both pliability and location during the fertile window. It also produces different types of mucus throughout the cycle and makes what we call ‘fertile fluid’ around ovulation. The cervix also undergoes major changes during pregnancy, as it fills with mucus that forms a plug to protect the fetus from the outside world. Near the end of pregnancy, the cervix begins to soften, the plug falls out and dilation occurs allowing birth to take place.
When it comes to predicting, most women will consistently find that there is about a 14-day gap between ovulation and the first day of menstruation (flow). This is called the luteal phase. Shorter cycles typically vary in the front half of the cycle, called the follicular or proliferative phase, because this is the phase of the cycle when the eggs (follicles) grow in preparation for ovulation, and the lining thickens in preparation for possible implantation.
Monitoring for ovulation
These days, there is an abundance of options for monitoring for ovulation. The truth is, many of them lead to a great deal of confusion and missed opportunities. Let’s review a few of the most common ovulation tracking methods and talk about the most underappreciated method for knowing when you’re ovulating for sure.
Apps: if you work with me in person or virtually, you know that I’m no fan of apps or other programs that tell you when you're ovulating. Here’s why: apps are taking an average of your last several periods and estimating when you are ovulating based on probability. The problem with this is that many women have irregular and somewhat unpredictable periods, which means that ovulation can vary by several days. If you have a totally predictable cycle, you don’t need to worry about using a tracking app, just subtract 14 days from the last day of your cycle (the day before your period starts) to accurately predict when you’ll ovulate next month.
BBT Charting: basal body temperature charting involves taking your temperature with a digital thermometer at the same exact time every morning, upon waking, and before getting out of bed or moving around too much. This method plots changes in your baseline temperature, depending on the phase of the cycle, with an expected dip just before and an expected rise just after ovulation. While I don’t usually recommend BBT charting as the primary method of fertility tracking (due to the challenges of daily temperature taking, among other things), it can be a useful diagnostic tool for people with irregular cycles or suspected issues with the luteal phase. It’s also used in Chinese medicine diagnosis to confirm certain patterns that inform choices in acupuncture and herbal protocols.
OPK: Ovulation predictor kits are urine tests that tell you when you’re most fertile by detecting your LH surge. LH (luteinizing hormone) is released by your pituitary gland once your follicles are producing enough estrogen to tell your brain that the lead follicle is ready to release. Upside: these tests can be very precise in determining your most fertile days. Downsides: women often miss the surge and thus their most fertile days, and the kits themselves are quite expensive, especially when used for many months. Women with PCOS may also experience LH surges in the absence of ovulation, so this method should be avoided if you have this condition.
You’re Cervix itself! Like so many structures in our wondrous bodies, the cervix is an amazing structure that plays a key role in your fertility. The two primary ways that the cervix can inform your fertile window is through changes in cervical mucus and changes in the cervix itself. Let’s look at each of these separately:
Cervical mucus: from roughly the end of your period through the day you ovulate, your cervix will make mucus that transitions from a substance that is inhospitable to sperm to a fluid that is not only a PH match for sperm, but that also contains little rivulets that make is easier for sperm to make its way to the egg. You can assess your own cervical mucus by placing a finger inside your vagina (once you are done bleeding), and taking a look! In the days leading up to prime fertility, you’ll notice that your vagina may be dry or slightly moist, with scanty mucus. After a few days, it will become more prolific and creamy white or slightly yellow. A few days before ovulation, you’ll notice that the mucus becomes transparent in color, more watery, and very stretchy. The best comparison is the color, transparency, and texture of egg whites. This is your fertile window! Estrogen is what produces fertile fluid, and younger women will tend to produce more and/or have more days of this type of discharge, which can range from just 1 day to up to 4-5 days. Your most fertile day will be the last day that your cervix produces this egg-white substance, so it’s a good idea to get to know your body well enough to recognize how many days of fertile fluid you make, and when it stops. Keep in mind that working with an acupuncturist and taking certain herbs and supplements may increase and optimize your cervical secretions over time. It’s also important to note that yeast infections, bacterial vaginosis, and even sexual arousal can make assessing cervical mucus confusing.
Your Amazing Cervix! In addition to changes in the fluid itself, the actual structure of your cervix changes throughout the menstrual cycle. Specifically, at the beginning of your cycle, the cervix remains closed, firm in texture, dry in fluid, and tilted back towards your bum. As you move into your fertile window, the cervix begins to tilt forward, moves higher in the vagina, and becomes very wet, eventually producing the transparent fertile fluid you’ve been waiting for. Once ovulation is complete, the cervix returns to its low, closed, and dry state, awaiting the signal of a pregnancy or the onset of another period. Isn’t that cool??
Understanding the cyclical nature of your cervix and the way those changes inform your most fertile days is, in my opinion, the most important and accurate way to optimize your chance of conceiving,
I’ll be going live on my private Facebook group on Monday 1/18/21 at 11 am to talk about all things cervix and to answer any questions you may have. I hope to see you there!
xo Laura
Owner/ Founder
Mother Nurture Wellness